Training the unstable client
I began training Amy* 8 years ago. She came to me because she wanted to build strength and prevent her osteoporosis from getting any worse. I was a much greener trainer at that point, and did my best to challenge Amy with heavier weight, dynamic movements, and body weight exercises. This didn’t go so well, and it became obvious that Amy was unable to support heavier weights, particularly in her upper body. Her shoulders were sloppy, and she didn’t have the ability to perform the movements in a technically proficient way. She also had some instability in her hips, and would occasionally get hip pain.
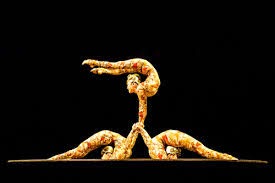
My first three years with her was a lot of trial and error to figure out what wouldn’t bother her shoulders and her hips, but would still give her strength (some of my clients are amazingly patient people. Why she stuck with me, I will never know). It wasn’t until I began studying joint position and mechanics and actually understanding how that impacted function that I was able to help her. Instability is rampant in the yoga world; to be good at many of the advanced postures requires quite a bit of mobility. While this should be balanced with an equal amount of strength, it is not unusual for people that already possess a large amount of mobility to gravitate towards the practice. Unless they spend time focusing on finding strength in each asana, this can be detrimental and lead to a lack of cohesive movement. The body will move in a way that lacks underlying support- it’s like removing the foundation of the house and hoping that the beams are strong enough to hold up the roof.
To understand the importance of joint stability, it is important to have a brief understanding of how the nervous system works. When we want to lift our arm, for example, the brain sends information via motor neurons to the appropriate muscles required to both stabilize the body for the action and to the muscles that lift the arm. Inside the joints are sensory nerve fibers that provide information to the brain about forces exerted on the joint tissues, joint position, and whether or not the joint is moving (Grubb, 2004). The nerve fibers that provide this information are called proprioceptors, and are located in the joint ligaments. This poses a problem when a person has joint laxity, or ligaments that are overstretched. In the shoulder, for instance, it is believed dynamic ligament tension is involved in signaling how much force the rotator cuff muscles need to exert on the humeral head (Kelly, 2002). If the ligaments lack tension, this would alter the activity of the 4 muscles of the rotator cuff, as well as decrease the stability of the joint simply because the ligaments aren’t doing a very good job keeping the shoulder in the socket. In a healthy joint, full range of motion should be pain free, the person should know where his arm (or hip, or ankle) is in relation to his body, and there should not be a fear that something is going to “slip” or “fall out,” common descriptors when you work with hyper mobile clients. It has been my experience that when someone falls into the category of hyper-mobility, it is important to change the training strategy to give stability on the deepest level.
In the case of Amy, she returned one summer from travel with shoulders that were not in a very good position. They were painful, her neck was overactive, and she said she couldn’t figure out “where they [the shoulders] are supposed to be.” At this point, I suggested we back off the weights for a while and try and a different approach. She agreed, and while it was frustrating at times, (“why is this so hard? I am not doing anything”), we progressed slowly and steadily. I gave her things to be aware of when she wasn’t with me, such as how to move from the scapula rather than the shoulder to reach for things. We worked on other things as well, such as breathing and improving her thorax/pelvis integration, and eventually we got back to weights, though I don’t have her go very heavy (she is 64, and I find it is better to train smart with older clients, rather than harder). She said to me last week, “thank you. My shoulders haven’t given me trouble in a very long time, and I feel way more stable.” Sometimes, people need mobility, sometimes they need strength, and often they need a combination of the two. We tend to avoid the things we aren’t good at; these are frequently the things we need the most. Having a little patience and an overall plan can go a long way in improving function and well-being.
Yours in health and wellness,
Jenn
P.S.- For a glimpse of some of the things I use to enhance shoulder stability, view the link here: https://www.youtube.com/watch?v=pmY8J2EVxuM
Grubb, B.D., (2004). Activation of sensory neurons in the arthritic joint. Novartic Found Symposium, 260, pp. 28-36.
Kelly, I. The Loose Shoulder, Maitrise Orthopedique, 111.