Hip stability, shoulder mobility
There is a test that is frequently used in clinical settings to diagnose hyper mobility disorders (Smits-Engelsman et.al, 2010). Typically, 5 different joints are tested and a score is assigned, which is known as the Beighton score. 9 is the maximum score, and the closer someone gets to 9, the greater chance they have joint laxity.* These are not people that need mobility work. Then there’s me. I score a 0, making the risk of me hyperextending anything pretty much impossible, barring some crazy accident where extremely high amounts of force place me into a pretzel like shape. I do not bend easily, and all the bend that I do have has been earned through years of yoga (I hear the cringing now), followed more recently by finding strength in end range positions. One of the benefits to lacking large amounts of mobility is I notice when something actually moves a little more easily. I also love the connections that exist between the structures of the body, primarily how something seemingly unrelated can have a deep impact on another area. And so I was excited on several levels when my morning movement practice allowed me to dramatically improve my shoulder range of motion through a hip strengthening flow.
In all honesty, the shoulder and hip connection isn’t exactly new. DNS explores the connection between the shoulder and hips via the anterior oblique chain. PRI views the relationship using the lens of reciprocal, alternating motion and common patterns that inhibit the ability of the right shoulder and left hip to work together during phases of gait. The fact that there is a relationship between the shoulders and hips isn’t news; how to best tap into this relationship, however, is something that merits exploration.
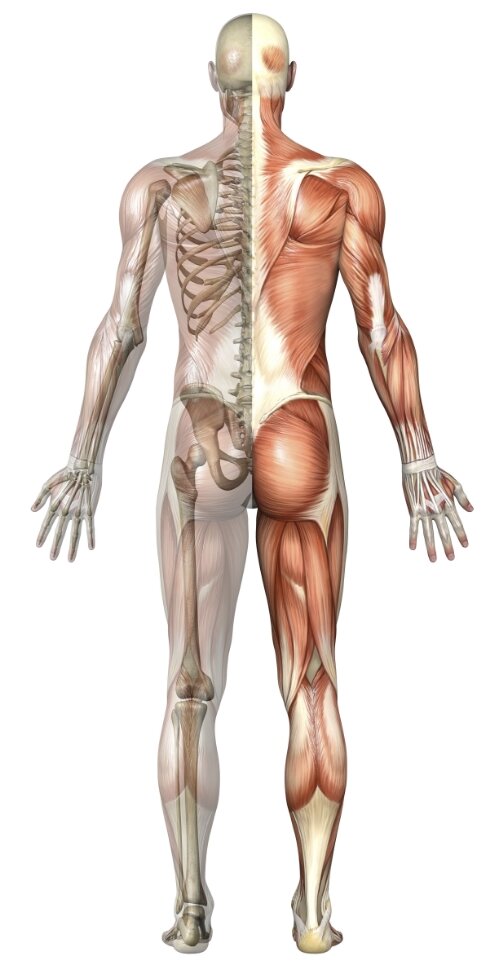
Researchers have studied how the hip and shoulder relate to one another through shoulder injuries in overhead athletes. Scher, et.al, found a relationship between the glenohumeral joint rotation in a professional pitcher’s dominant arm and contralateral hip internal rotation. A lack of hip internal rotation correlated to decreased total glenohumeral joint ROM in pitchers with a history of injury. (Interestingly, these researchers found the strategy professionals use to pitch is different than college level pitchers and high school pitchers. Food for thought for a different post on motor control and efficiency). The researchers point out it is just as likely the decreased hip internal rotation causes the decrease in shoulder ROM as it is the shoulder ROM causes the decreased hip internal rotation. In other words, there really isn’t any good way for a professional in the movement field to know which is the primary driver for injury, and while it is possible a good clinician could figure that out, that is outside the scope of this blog. What matters is the relationship, and the ability of force to be distributed from the hip to the shoulder or vice versa, depending on the movement goal. This fits in neatly with the idea that force is transmitted in a non-random way based on body position. Examples of this abound with some of the myofascial chains that have been suggested. In fact, recently, Wilke, et.al, performed a fairly comprehensive analysis of the existence of myofascial chains. They concluded there is strong evidence supporting the superficial back line, back functional line, and the front functional line, with moderate to strong evidence supporting parts of the spiral line and the lateral line. How does this support the hip and shoulder relationship?
The spiral line, which is also a foundation for several of the DNS positions, runs from the head to the feet (Boser and Lesondak, 2010). Specifically, it moves from the splenius captius to the rhomboids and serratus anterior, which joins with the external obliques and rectus abdominis on one side. From there, it crosses to the opposite internal oblique, anterior TFL and IT tract down to the lateral tibial condyle and tibialis anterior. The functional back line consists of the latissimus dorsi, gluteus maximis, and vastus lateralis, while the functional front line is comprised of the pectoralis major, rectus abdominis, and adductor longus. If you aren’t an anatomy geek and are getting a little bit lost with these latin words my spellcheck doesn’t like, the thing all of these chains have in common is muscles that influence the shoulder joint are connected via abdominals to muscles that influence the hip joint. Quite simply, if you want to improve shoulder function, you need to look at abdominals and hips. If you are doing any concentrated hip and/or shoulder work, abdominal engagement is necessary and will enhance the shoulder and hip connection, especially if you respect position by having a ZOA as a frame of reference.
So how can this be put into practical application? I have used variations on the hip sequence below** on three people and have found improvements in shoulder mobility directly afterwards in all of them. This, of course, is a small sample size and not by any means a controlled setting for testing, but the correlation is significant enough I decided to continue using variations of this in their programming. In fact, one reported implementing the hip work seemed to clear up a long time issue he had been having with his latissimus on the right side. If you look at the anatomy, this isn’t all that surprising. Load can be dispersed in a more fluid way up the functional back line. (It is worth noting these three are similar to me in that they aren’t hypermobile. That would require a different sequence with an emphasis on stability). If I can free up overhead movement and improve general ease and strength in the upper extremity, why wouldn’t I want to do that? For my own movement practice, the improvement in pull-ups and rope climbing ability increases directly following hip mobilization and activation. Once I made this correlation, I capitalized on it. The more aware you can become of how your body moves, the more in tune you will be when things become easier or harder. The same is true of clients. While nothing works for everyone, if you or one of your clients score low on the Beighton scale and feel restricted in overhead movement, it wouldn’t hurt to work on hip mobility and stability with an awareness of abdominals. If it helps overhead mobility, great, and even if it doesn’t, chances are pretty good the hips will feel a renewed sense of freedom.
Yours in health and wellness,
Jenn
*Tony Gentilcore wrote a good blog on hyper mobility and the Beighton score, which can be found here: http://tonygentilcore.com/2014/11/stretching-isnt-always-answer-3-common-mistakes/
**Variations of some of the exercises I have been using can be found here: https://youtu.be/g2Rd4roRC2M and https://youtu.be/82CsHMI0l1M
(I am constantly tinkering, so this isn’t the end all be all. It is simply to offer some ideas).
**The ELDOA method utilizes the idea of fascial chains in a really interesting way. The book, “The Permanent Pain Cure,” by Ming Chew has a very thorough description of some of the stretches in the ELDOA method. These are not easy, and I personally think stretch is a bit of a misnomer because they are quite active in nature- more like an isometric strengthening exercise. I am pleased with how they work and have enjoyed implementing them in several clients’ programming. If you are curious about fascial stretching, this is a worthwhile reference.