Resources Blog
Embodied Perspectives: Holistic Fitness, Movement, and Mindfulness Resources
The Embodied Perspectives blog explores the intersection of holistic fitness, movement, and mindfulness, offering insights into how we move, why it matters, and how awareness shapes our well-being. Through research, practical applications, and personal reflections, this blog provides a deeper understanding of movement’s role in strength, mobility, and overall health. Whether you're a movement professional, an athlete, or someone seeking a more mindful approach to fitness, you'll find thought-provoking discussions and actionable ideas to enhance your practice.

Spiraling Strength: A Shoulder Flow for Mobility and Ease

Play with Your Overhead Reach

A 2-Minute Exploration: Shifting Weight from Hands to Feet

Morning Flow: Leading with the Xiphoid Process

Is sitting in a deep squat the best way to improve it?

Why Your Flexibility Isn’t Improving—And What the Pelvic Floor Has to Do With It

Explore Spinal Intelligence: Three Ways to Approach the Seated 90/90 Position

Toes to Bar: Leg Exercise or Arm Exercise? How to Train for Different Outcomes
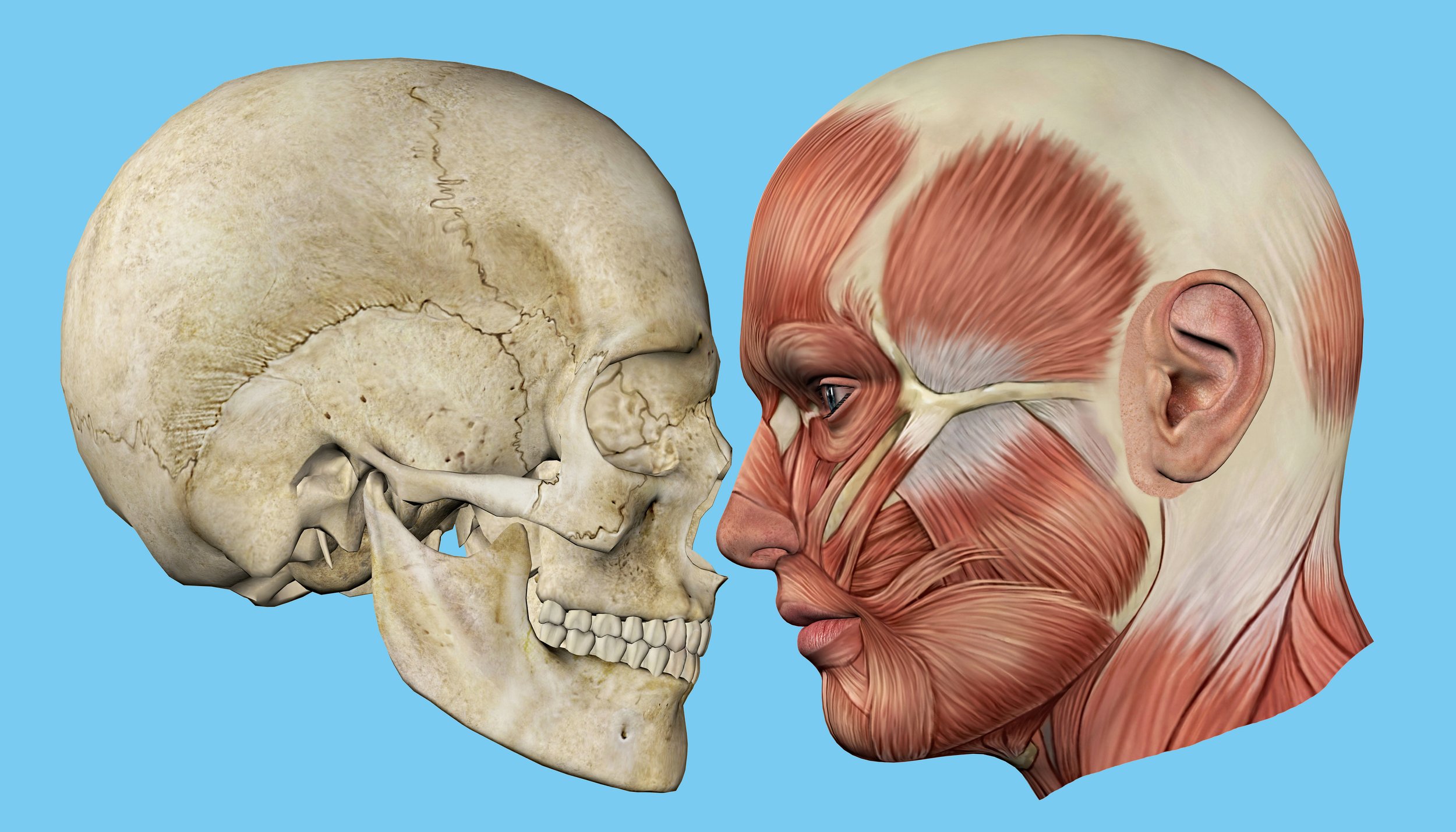
My Visit to the Dentist: A Type A Perspective on Relaxation and Jaw Exercises

Mindfulness, movement, and exercise season 2 episode 7: BDNF and learning

Exploring body connections: Pelvic floor and feet
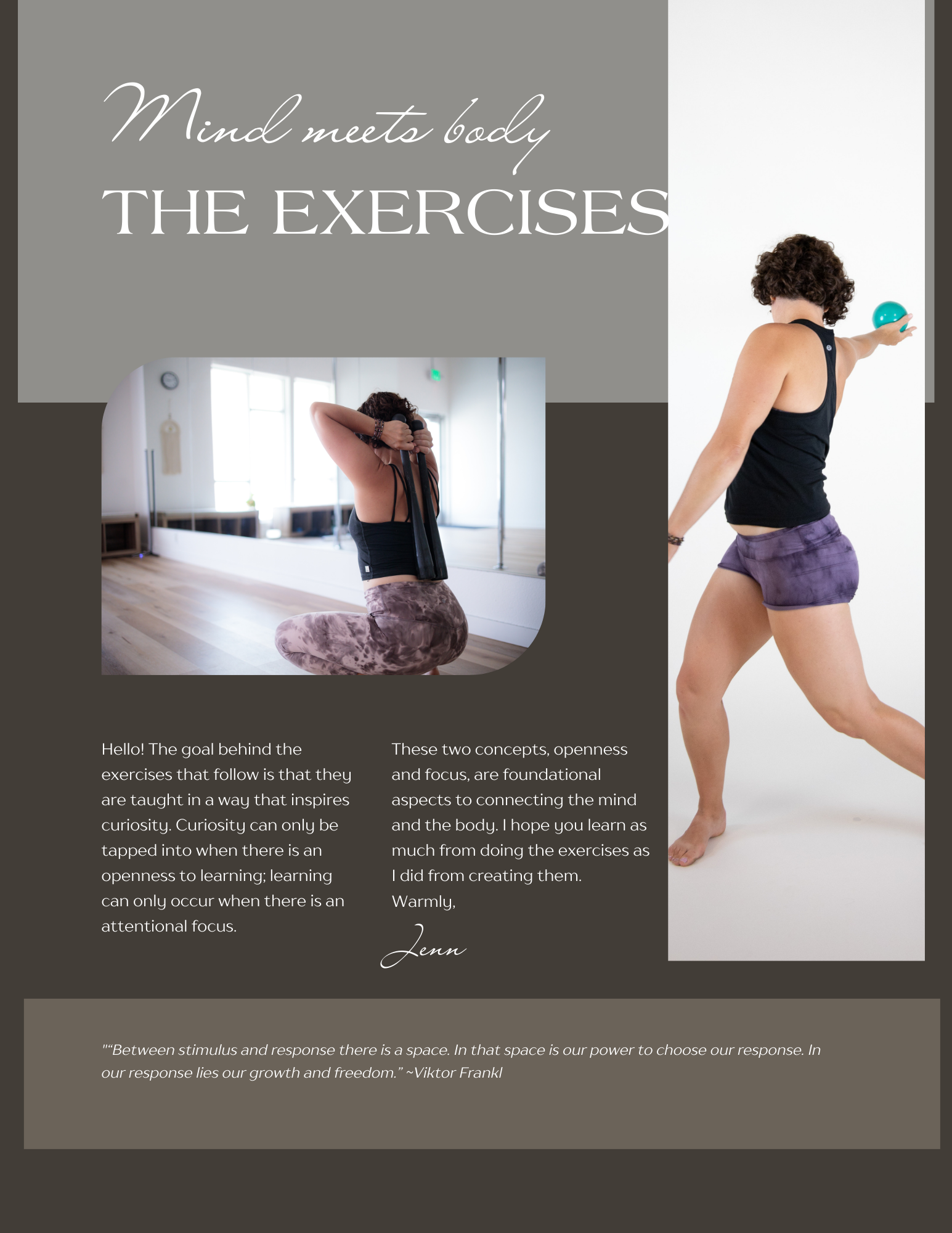
Mind Meets Body: The program

A story about stress

The Cossack Squat

Pressure, tendinopathy, and movement

Resistance and Change

Levers and Movement
Maps and movement

Pole dancing and book publishing


